Diabetic Skin Issues: A Primer
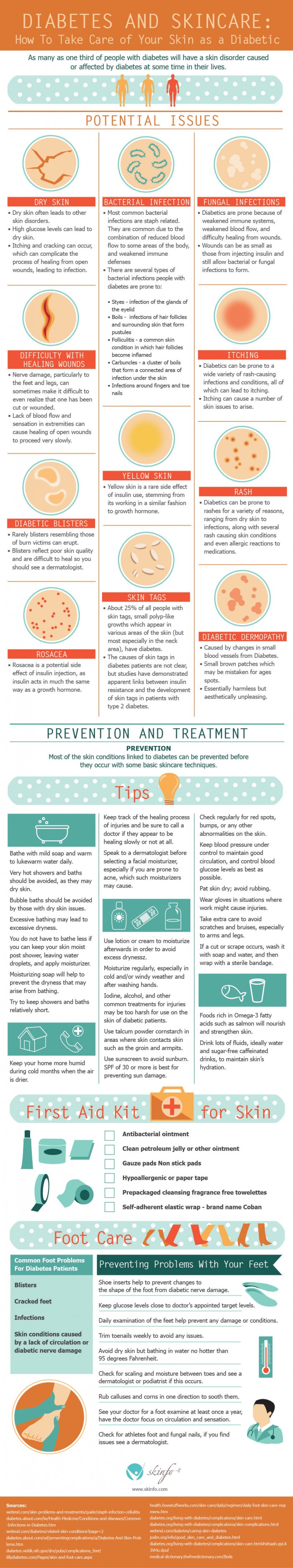
Diabetics expect to learn the basics of insulin, blood sugar, and glucose- but what many diabetics may be surprised to learn is that as many as one third of people with diabetics will have diabetic skin issues caused or affected by their disease at some point in their lives.
These skin issues and disorders often stem from the typical side effects of diabetes. For example, high glucose levels can cause dry skin, which often causes other skin disorders such as rashes, itching, cracking, and difficulty healing from open wounds.
Similarly, many diabetics experience reduced blood flow to some areas of the body and weakened immune defenses, which can lead to bacterial infections or fungal infections. Weakened immune systems, reduced blood flow, and difficulty healing from open wounds can also lead to fungal infections.
Fortunately, most of the skin conditions correlated with diabetes can be prevented by following basic skincare procedures. Diabetics should bathe daily in warm water, using moisturizing soap and lotions afterwards to prevent dryness.
Diabetics should also be aware that iodine, alcohol, and other common treatments for injuries may be too harsh to use on their skin. To strengthen skin, diabetics should include foods rich in omega-3 fatty acids in their diet and drink plenty of water.
Diabetics can also stock their cabinets with first aid kits compiled specifically for treating skin issues. This kit could include:
- Antibacterial ointment
- Clean petroleum jelly
- Gauze/non-stick pads
- Hypoallergenic tape
- Prepackaged cleansing fragrance-free towelettes
- Self-adherent elastic wrap from Coban
Finally, diabetics should be aware that skin issues can go all the way from head to toe- literally. Diabetics often encounter foot problems such as blisters, cracked feet, infections, and skin conditions caused by a lack of circulation or diabetic nerve damage. Head these off by seeing your doctor for a foot examination annually that focuses on circulation and sensation.